Sep 27, 2023 | Southern Arizona
Aside from skin cancer, prostate cancer is the most common cancer in men. Therefore, it’s important to learn some facts about prostate cancer screenings and make sure you, or the males in your life, are getting screened for prostate cancer in a timely manner.
Early Detection of Prostate Cancer Can Provide Better Outcomes for Patients!
All men, even healthy ones, can benefit from making prostate cancer screenings part of their regular healthcare routine. Doctors sometimes recommend testing simply because of age or family history. Other times, patients have some symptoms, and their doctor may suggest a prostate cancer screening as the first step to understanding the problem. Below is some information that can help you know when it’s the right time to get screened.
1. When Symptoms are Present
Sometimes men experience symptoms associated with prostate cancer, but those same symptoms can also occur in non-cancer-related conditions such as an enlarged prostate (“BPH”). When a patient visits their general practitioner or urologist with concerns, a prostate cancer screening is a very common part of the diagnosis process — even if the diagnosis isn’t cancer.
2. When You Have a Family History of the Disease
Between 5-10% of prostate cancers are hereditary. Men are at risk of developing prostate cancer if another male in your family has been diagnosed with prostate cancer previously. Several newer genetic tests, such as the PHI (Prostate Health Index), 4KScore, and PcA3, seem to be more accurate than the PSA test, your doctor may recommend one of those as well.
The American Cancer Society suggests screening for men over 50 years old if they have one family member who was diagnosed with prostate cancer at a relatively young age (under 65 years old). Men with two or more family members who developed prostate cancer should be screened once they reach the age range of 40 to 45. Also, African American men have a higher risk of developing prostate cancer, and the ACS recommends that they be screened beginning at the age of 45.
3. When You Turn 50
Prostate cancer treatments have a much higher success rate when found at an early stage. This is why prostate cancer screenings are regularly done on patients who have no symptoms or immediate family history of prostate cancer. The American Cancer Society (ACS) recommends screening for men over the age of 50 who have no unusual prostate cancer risk factors.
It’s important for men to talk with their doctors to make an informed decision on when they should start prostate cancer screenings. After the initial screening, their doctor will also make recommendations on how often to continue follow-up screenings.
To learn more about prostate cancer screenings, ask your doctor for a referral to your local prostate cancer specialists. If you are located in Arizona and would like to make an appointment with one of Arizona Oncology’s prostate cancer specialists please contact us for an appointment. With cancer treatment centers located throughout Arizona, you’ll find advanced and personalized treatment, expert guidance from our specially trained and board-certified oncologists, and leading-edge cancer research options.
Originally posted in 2018, updated in 2024.
Sep 26, 2023 | Southern Arizona
By Robert Gin, MD
The word profiling has been defined as the use of personal characteristics or behavior patterns to make generalizations about a person. Profiling is used in our everyday lives. When someone knocks on our door and we look through the peephole, we make a split decision on the person’s appearance to decide if we open the door or turn off our lights to show no one is at home. Dating sites and the internet collect data and use that information to present users with a compatible person or products. However, profiling is not limited to just people. Think about walking along the sidewalk and you see a pit bull (no offense to pit bulls).
Some of us may be intimidated and decide to walk across the street. Or you go to the supermarket, and the closest parking space is next to a car with big doors or has lots of dents. You may decide to park a little farther to keep your car dent free.
In oncology, profiling has been around for quite some time. A good example is estrogen receptors for breast cancers. In 1896, it was noted that removal of ovaries in premenopausal women with advanced breast cancers led to regression of their cancer. However, only about 30% of women responded after removal of the ovaries. Even though this relationship between estrogen and breast cancer was known, it was not until the mid-1970s when a test was developed by breast cancer researchers to detect estrogen receptors on cancer cells that allowed them to respond to estrogen ablative therapies. As a standard of care, all breast cancers are tested for these receptors to determine if they will benefit from removal of the ovaries to taking a pill for the next five to ten years.
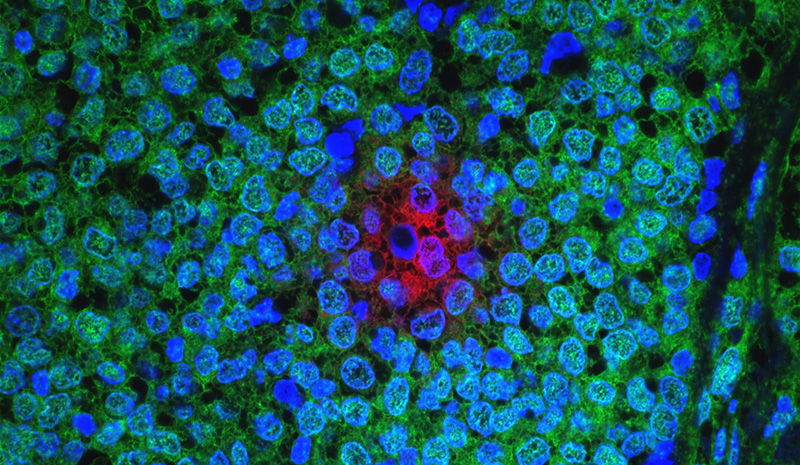
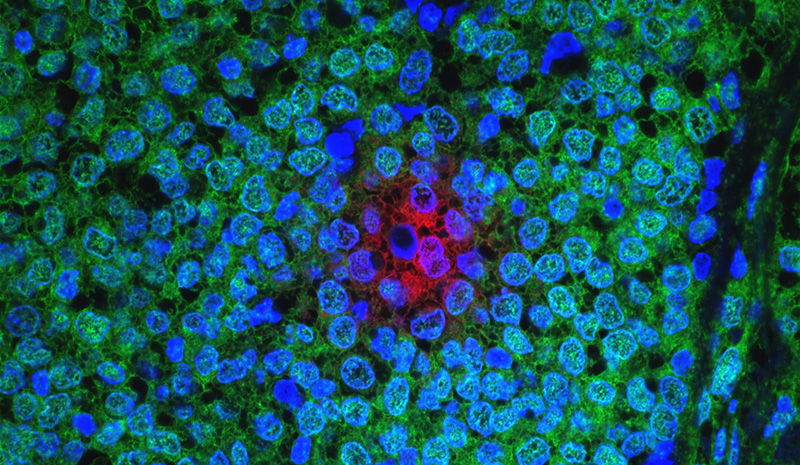
Much has changed since 1970. With advances in medical knowledge and technology, profiling has extended beyond testing for hormone receptors. Profiling now looks at the mutated genes of the tumor cells. These genes instruct cancer cells to grow, to spread, form blood vessels, become more aggressive, and hide from the body’s immune system. By understanding the behavior of these mutations, we can apply appropriate targeted and molecular therapies.
A widely-used test to profile breast cancer is the Oncotype DX. By analyzing 21 genes, this helps the oncologist determine if an early-stage breast cancer is harboring aggressive behavior to spread, (what I call a wolf in sheep’s clothing), and would benefit from chemotherapy. For all cancers, profiling can provide the physician with gene-specific information about the tumor and can assist in deciding which chemotherapy drugs could be most effective against them. Some mutations allow a cancer to hide from the body’s immune system. Profiling can detect these mutations and allow the oncologist to use immunotherapy drugs to “unmask” these tumors and allow the body’s own immune system to target the tumor.
In summary, most cancers are best treated by standard of care guidelines. For now, molecular profiling can provide information to your oncologist regarding the necessity of chemotherapy for early-stage breast cancer. In instances of rare cancers or those that have not responded to standard cancer treatments , profiling can aid the oncologist in choosing the best therapy for that cancer.
Originally posted in 2017, updated in 2024.
Robert Gin, MD, is a Radiation Oncologist at Arizona Oncology in Tucson. He received Bachelor of Science degrees in Chemistry as well as Molecular and Cellular Biology, with a minor in math and physics, from the University of Arizona, where he also completed his residency in Radiation Oncology, serving as Chief Resident.

Aug 25, 2023 | Southern Arizona
Arizona Oncology proudly announces its participation in the Enhancing Oncology Model (EOM), a novel program aimed at improving cancer care. Only 44 oncology practices across the country, including ours, have been selected to take part in this initiative. Backed by the Center for Medicare and Medicaid Innovation (CMMI), the program aligns with the Biden Administration’s Cancer Moonshot effort to enhance the cancer treatment experience.
What EOM Means for Patients
The EOM primarily targets Medicare and Medicaid patients undergoing chemotherapy for seven cancer types: breast cancer, chronic leukemia, small intestine/colorectal cancer, lung cancer, lymphoma, multiple myeloma, and prostate cancer. Patients being treated for these conditions at Arizona Oncology can expect the following benefits:
- Round-the-Clock Clinician Access: Easy access to appropriate clinicians and seamless communication with your oncologist and care team between appointments, all aided by real-time access to medical records.
- Personalized Support: Enhanced services like patient navigation, tailored to provide guidance throughout the cancer treatment journey.
- Tailored Care Plans: Detailed care plans aligned with patient preferences, encompassing prognosis, treatment options, symptom management, and overall health needs.
- Social Assistance: Help with health-related social needs, including food and transportation through https://usoncology.findhelp.com/.
- Feedback Platform: Opportunities to share feedback on the cancer care experience and health outcomes.
Aim of EOM: Improved Patient Care
EOM’s core objective is to enhance care coordination and elevate patient outcomes. By focusing on individual patient needs, the program aims to provide better support during cancer care, promote clearer understanding of diagnoses, and facilitate collaborative treatment planning with oncologists.
Connect with Arizona Oncology
Our involvement in EOM stems from our commitment to supporting patients and refining their care experience. This initiative allows us to maintain comprehensive, coordinated care while intensifying our efforts to identify and address health disparities. Arizona Oncology remains dedicated to prioritizing patient care as we embrace EOM. Together, we’re embarking on a journey toward improved oncology care, focused on practicality, innovation, and an unwavering commitment to helping our patients thrive with and beyond cancer.

Aug 3, 2023 | Southern Arizona
Exposure to ultraviolet light is the primary cause of melanoma and nonmelanoma skin cancers and premature aging. Both of these can be largely avoided by protecting the skin from ultraviolet rays – whether from the sun or tanning beds. If you’re going to be outdoors one of the best things you can do to protect your skin is to wear sunscreen. Wearing protective clothing and avoiding the sun at the hottest times of the day (10 am – 4 pm) can also reduce the risk of developing skin cancer.
With so many options, numbers and phrases on sunscreen packages, going to the store to choose the one that’s best for you can be overwhelming. Here are some things to help you understand what you’re reading on a sunscreen label.
Your Checklist for Choosing Sunscreen
- Choose the type of sunscreen you will apply. Sunscreen options include lotions, sprays, sticks, and gels. It is easiest to ensure where you are applying sunscreen with lotions, sticks and gels so that areas do not get missed. Sunscreen sprays are popular and convenient; just be sure to avoid spraying into eyes, nose and mouth and apply generously.
- Choose a high enough SPF. The sun protection factor (SPF), in a product ranges from 2 to 100 and refers to how much of the sun’s UVB rays are blocked.
- SPF 15: Block 93% of the sun’s UVB rays
- SPF 30: Blocks 97% of the sun’s UVB rays
The American Academy of Dermatology recommends wearing sunscreen with SPF of 30 or higher.
- Select a broad spectrum sunscreen. The sun generates both ultraviolet (UV) A and B rays. UVA rays cause premature aging of the skin (wrinkles and age spots.) UVB rays cause sunburns. Both UVA and UVB rays can contribute to skin cancer and your sunscreen should include protection from both.This might also be called “broad spectrum” sunscreen. A sunscreen that does not say “broad-spectrum” only protects skin from UVB (burning) rays.
- Identify the active ingredients you prefer. Sunscreens come in two different categories: barrier vs absorption
- Barrier sunscreens, like titanium dioxide and zinc oxide, put a layer of protection between the sun and your skin that deflects the sun’s rays. This is often available in a white, thick cream or stick.
- Chemical sunscreens absorb the sun’s rays which often use active ingredients oxybenzone or avobenzone.
- Remember that water resistant is not waterproof. “Water resistant” and “sweat resistant” mean the same thing on a sunscreen label: these sunscreens have been proven to remain effective for at least 40 minutes while you’re in the water or sweating. You have to reapply when you get out of the water to prevent sunburn.
Prior to heading outdoors, whether it’s all day or just running errands in your car, apply a broad-spectrum sunscreen of at least SPF 30 (and water/sweat-resistant for swimming or activities) 20 minutes beforehand. Then, you will enjoy the great outdoors with peace of mind that you’re reducing your risk of skin cancer. And don’t forget to reapply every 90 minutes to two hours and after swimming or sweating.
Originally posted in 2017, updated in 2024.

Jul 20, 2023 | Southern Arizona
According to the American Cancer Society, about 2 million new cancer cases are expected to be diagnosed in 2024. More than 18 million Americans will be living beyond cancer. The American Cancer Society reports a majority of cancer survivors (69%) were diagnosed 5 or more years ago.
Prostate, breast and colorectal cancers are the most common diagnoses among survivors. The increase in survival rates over the last 5 years can be attributed to early detection methods for cancer screening, and advancements in identifying new targeted cancer therapies. As cancer detection and treatment continue to improve on disease free survival, it is estimated that there will be 26 million survivors by 2040.
Who is a survivor?
There are many definitions of a cancer survivor but most agree that an individual is considered a cancer survivor from the time of diagnosis through the balance of his or her life. The cancer patient generally moves through three distinct phases.
- The first phase, often the shortest, is from diagnosis to the completion of initial cancer treatments. To cure cancer or to extend quality of life requires intensive oversight of the patient and accompanying symptoms and side effects. This phase is frequently the most physically and emotionally distressing for patients to navigate and results in heavy reliance on healthcare professionals and one’s support network.
- The second phase transitions the patient from treatment to extended survival with evidence that the disease is responding to treatment. During this phase, cancer survivors may worry, fear a recurrence, or develop a feeling of isolation as they transition out of active cancer therapy and into surveillance. Imaging, laboratory studies and appointments become less frequent and patients may be prescribed additional therapies to prevent the recurrence or spread of the cancer.
- The final phase constitutes long term survival. Patients may see their oncologist annually or be followed by their primary care physician. Patients may or may not continue to take medications to minimize recurrence.
Most cancer patients are ecstatic when they complete active treatment. Patients were educated about what to expect during chemotherapy, after surgery or with radiation. They were reassured that all efforts would be made to minimize side effects during treatment. Unfortunately, as a health profession, we haven’t done a great job in preparing the patient about what to expect once this phase is completed.
In 2005, the Institute of Medicine and the National Research Council released the report “From Cancer Patient to Cancer Survivor: Lost in Transition” which highlighted gaps in the care for cancer survivors and recommendations for survivor- ship care. Many survivors experience physical, emotional, and psychosocial effects of cancer and it treatment. Fortunately, oncology practices have started responding to the unique needs of survivors and are now focusing on survivorship as a distinct entity of cancer care.
It is imperative that survivors continue to follow cancer screening recommendations, practice healthy habits, and meet regularly with their primary care physician.As a cancer patient moves further away from active treatment, it’s difficult to remember all the treatments and studies one has undergone. Patients completing primary treatment are provided a comprehensive care summary and follow-up plan with healthy maintenance recommendations written by the primary oncology provider(s). It is a useful tool that patients can refer to throughout the remainder of their lives and provide to their providers.
Cancer survivors are at risk for side effects from treatment that linger such as neuropathy, fatigue and memory problems. Survivors are also at risk of effects that can develop months to years after treatment such as osteoporosis, infertility, heart problems, and second cancers. Each patient’s risk profile is unique and directly related to their health status, family history and the types, as well as duration of treatments.
Survivors need to focus on wellness, diminish the effects of cancer and control any personal comorbidities such as diabetes, obesity and heart disease. It is imperative that survivors continue to follow cancer screening recommendations, practice healthy habits, and meet regularly with their primary care physician.
Being a cancer survivor is a lifetime commitment to living well and minimizing risks. Many survivors, their families and friends thought that once treatment was over, life would revert back to the way it was before a cancer diagnosis. Survivors find that there is now a new normal which involves negotiating roles with families, friends and employers, making lifestyle modifications and coping with fluctuating emotions. Cancer survivors, empowered and partnered with their providers, are emerging from their cancer journey more resilient than ever.
Originally posted in 2017, updated 2024.

Jul 18, 2023 | Southern Arizona
Ways to Minimize Side Effects from Cancer Treatment
Because of advances in cancer treatment, more and more people can expect to reach remission or to live a long life with cancer. This is wonderful news! However, going through cancer treatment often isn’t easy. Cancer medications and radiation treatments can cause a variety of side effects that can be difficult to deal with. Here are some things you can do at home or with the help of your doctor to minimize side effects from cancer treatment.
Appetite Loss. People being treated for cancer often don’t feel hungry. But when you don’t get enough nutrients, you can become weak, dehydrated, or lose too much weight. If you are experiencing appetite loss from cancer treatment, try these tips:
Drink lots of liquids. If eating a full meal seems too much, opt for smoothies, healthy shakes, broths, and plenty of water.
Choose high-nutrient foods. If you are eating less, it’s more important than ever to focus on healthy, nutrient-dense foods that are high in protein and calories. Fruits and vegetables as well as whole grains are good choices, along with modest amounts of meat and dairy products. Arizona Oncology offers nutrition services to help with appetite loss and other nutritional issues during cancer treatment. Talk to your treatment team for more information
Eat your biggest meal when you are most hungry. If you don’t ever feel hungry, try eating several small meals or snacking throughout the day.
Bleeding and Bruising. Some cancer treatments make you more prone to bruises or bleeding by lowering the platelet count in your blood. Some things you can do to reduce your risk of bruising or bleeding include:
Avoid certain medications. Common, over-the-counter medications that increase bleeding risk are ibuprofen and aspirin. Your doctor can provide you with a more comprehensive list.
Brush your teeth gently. Make sure your toothbrush is labeled “soft”.
Use an electric shaver. This will avoid you nicking your skin with a razor.
Be extra careful. Take extra care when you are in the kitchen, doing sports, or working with tools.
Nausea and Vomiting. Feeling sick to your stomach or vomiting are common side effects of cancer treatment. Depending on what is causing the upset, your doctor may recommend one or more of the following steps:
Anti-nausea medication. Nausea and vomiting can be caused by different things, so there is not a one-size-fits-all approach. Your doctor will recommend a medication and let you know when and how often to take it. You may need to take the medication even on days when you don’t feel sick. Tell your doctor if you aren’t getting relief, because a different medication may work better for you.
Avoid certain foods. Greasy, fried, spicy, or sweet foods may make you feel sick. Eating foods cold can be easier on your stomach. Sometimes the smell of certain foods alone can upset your system. If this is the case, consider asking someone else to prepare your food.
Time your meals around your treatments. Pay attention to how eating before treatments affects you. For some people, a small snack before treatment helps calm their stomach, while others need to avoid eating before treatment altogether. Wait at least an hour after treatments before eating or drinking.
Complementary medicine. Acupuncture, deep breathing, relaxation techniques, hypnosis, and guided imagery are complementary practices that may help with nausea and vomiting. Ask your treatment team for more information on these services if you are interested in trying one of these therapies
Skin and Nail Changes. Radiation, chemotherapy, stem cell transplants, immunotherapy, and targeted therapy can all cause skin-related changes. Depending on the treatment type, these can show up as dryness, itchiness, irritation, rashes, or blisters. It is important to tell your doctor about any skin changes you experience. At home, the following tips can help minimize skin and nail issues related to cancer treatment:
Use mild soaps. Mild, fragrance- and dye-free soaps are best for irritated skin. Your nurse can recommend specific skin products.
Moisturize. Moisturize after showers while your skin is still wet. Your nurse can recommend specific moisturizers and ointments to deal with especially dry, irritated skin.
Use warm, not hot water.
Wear gloves.
Don’t get a manicure or pedicure during treatment.
Use medications for rashes if your doctor recommends them.
Insomnia. If you are having problems falling asleep or staying asleep during cancer treatment, you are not alone. Sleep problems can be a side effect of treatment or the result of medications, stress, or other factors. If your sleep issues are due to pain, urinary issues, or diarrhea, your doctor can help. You may also want to try some of the recommendations below:
Practice good bedtime habits. Avoid electronics at least two hours before bed. Keep your room cool, dark, and quiet. Don’t eat or drink a lot before bedtime. Get your exercise earlier in the day, not at night.
Cognitive behavioral therapy (CBT). If your thoughts are keeping you awake at night, a CBT therapist can help you manage negative thought patterns and calm your mind. Relaxation therapy. Guided imagery, muscle relaxation, and self-hypnosis can also help you get a good night’s rest.
Sleep medicication. Medication to help you sleep can be prescribed on a short-term basis if other strategies don’t work.
Having strategies to minimize side effects can help you feel more in control as you undergo treatment for cancer. Some side effects cannot be controlled, such as hair loss, but there are ways to cope with them. For more tips on dealing with side effects from your cancer treatment, visit https://arizonaoncology.com/cancer-treatment-tips/chemotherapy-side-effects/.
Page 7 of 18« First«...56789...»Last »