Sep 24, 2024 | Southern Arizona
September is Leukemia and Lymphoma Awareness Month, providing us with a perfect opportunity to dispel myths about these often misunderstood blood cancers. Below are some of the most common misconceptions:
1. Myth: Leukemia and Lymphomas Aren’t Cancer
Fact: Both leukemia and lymphoma are types of cancer. While many people think of cancer in terms of solid tumors, leukemia and lymphomas are considered blood cancers. They affect the production and function of blood cells, which are essential for overall health.
- Leukemia starts in the bone marrow, where blood cells are produced. The disease typically leads to the uncontrolled growth of abnormal white blood cells, which interferes with normal blood cell production.
- Lymphoma, on the other hand, affects the lymphatic system, a critical part of the immune system. There are two main types of lymphoma: Hodgkin lymphoma and non-Hodgkin lymphoma.
2. Myth: Leukemia Only Affects Children
Fact: While leukemia is often associated with children, especially in discussions about acute lymphoblastic leukemia (ALL), it’s important to know that leukemia also affects adults. In fact, certain types of leukemia are more common in adults:
- Acute myeloid leukemia (AML) is more prevalent in older adults. AML starts in the bone marrow, but most often it quickly moves into the blood, as well. It can sometimes spread to other parts of the body including the lymph nodes, liver, spleen, central nervous system (brain and spinal cord), and testicles. AML has many other names, including acute myelocytic leukemia, acute myelogenous leukemia, acute granulocytic leukemia, and acute non-lymphocytic leukemia.
- Chronic leukemias, such as chronic lymphocytic leukemia (CLL) and chronic myeloid leukemia (CML), primarily affect adults. Chronic lymphocytic leukemia (CLL) is one the most common types of leukemia in adults. It starts in early forms of certain white blood cells (called lymphocytes) in the bone marrow, then moves into the blood. In CLL, the leukemia cells often build up slowly. Many people don’t have any symptoms for at least a few years. Over time, the cells can build up and spread to other parts of the body, including the lymph nodes, liver, and spleen. Chronic myeloid leukemia (CML) is a type of cancer caused by a genetic mutation in myeloid cells in the bone marrow, leading to abnormal cell growth that can spread to the blood and other parts of the body, such as the spleen. CML is a fairly slow growing leukemia, but it can change into a fast-growing acute leukemia that’s hard to treat.
Similarly, lymphomas occur in both children and adults. The age of onset and the type of lymphoma can vary significantly.
3. Myth: Patients with Leukemia Just Need a Bone Marrow Transplant to be Cured
Fact: Not all types of leukemia can be cured with a bone marrow transplant, and not all patients are candidates. While a bone marrow transplant (also called a stem cell transplant) is an important treatment option, factors such as the type of leukemia (acute or chronic), the patient’s age, overall health, and the stage of the disease determine whether a transplant is the best option. Additionally, some leukemias respond well to other treatments and may not require a transplant.
Treatments for leukemia are tailored to the individual and may include:
- Watchful Waiting: People with chronic lymphocytic leukemia who do not have symptoms may be able to put off having cancer treatment. By delaying treatment, they can avoid the side effects of treatment until they have symptoms.
- Chemotherapy: Chemotherapy uses drugs to destroy leukemia cells. Depending on the type of leukemia, patients may receive a single drug or a combination of two or more drugs. Chemotherapy may be delivered in the form of a pill, via infusion, or directly into the cerebrospinal fluid.
- Targeted therapy: This includes drugs that specifically attack cancer cells based on their genetic makeup.
- Biological Therapy: Biological therapy for leukemia enhances the body’s natural defenses, using treatments like monoclonal antibodies to target and destroy leukemia cells or interferon to slow their growth in some cases of chronic myeloid leukemia.
4. Myth: Only Blood Relatives Can Be a Donor for a Bone Marrow or Stem Cell Transplant
Fact: While a relative may sometimes be a good match for a bone marrow or stem cell transplant, many patients find life-saving matches through unrelated donors. Global bone marrow donor registries, such as the National Marrow Donor Program (formerly known as Be The Match), have millions of potential donors. A match can come from anyone who shares similar genetic markers, even if they aren’t a blood relative. Ethnic diversity also plays a critical role, making it important for people from all backgrounds to register as donors.
Stem cell transplants from unrelated donors save lives every year, offering hope to patients who otherwise might not find a match within their family.
5. Myth: Only Older Adults Get Lymphoma
Fact: While non-Hodgkin lymphoma (NHL) is more common in older adults, Hodgkin lymphoma (HL) is often diagnosed in young adults, typically between ages 15 and 35. Both Hodgkin and non-Hodgkin lymphomas can occur at any age, but they differ in how they present and respond to treatment:
- Hodgkin lymphoma tends to have a high cure rate, even in advanced stages, especially in younger patients. It is characterized by the presence of large, abnormal cells called Reed-Sternberg cells, which are typically found in lymph nodes. Hodgkin lymphoma tends to spread in a more predictable pattern from one lymph node group to another.
- Non-Hodgkin lymphoma includes a wide variety of subtypes, some of which are more aggressive and may require more complex treatment. NHL includes a broader category of lymphomas that do not have Reed-Sternberg cells and can arise from either B cells or T cells (types of white blood cells). NHL can spread more randomly throughout the body, making it challenging to treat.
6. Myth: If Leukemia or Lymphoma Comes Back, There’s Nothing That Can Be Done
Fact: A recurrence doesn’t mean that there are no options left. Many patients who experience a relapse can benefit from second-line therapies, including clinical trials, new treatment protocols, or even a stem cell transplant. Advances in treatment are offering new hope for those facing recurrent blood cancers.
7. Myth: Leukemia and Lymphoma Always Develop Quickly
Fact: While some forms of leukemia and lymphoma, such as acute leukemias, develop rapidly and require immediate treatment, others can progress more slowly. Chronic leukemia, for example, may not require treatment right away and can be monitored for years before symptoms worsen.
8. Myth: A Healthy Lifestyle Prevents Leukemia and Lymphoma
Fact: The exact causes of blood cancer are not completely understood, but it is believed to result from a combination of genetic and environmental factors. Factors like smoking, exposure to radiation, and certain chemicals have been associated with a higher risk of developing some types of blood cancers. While a healthy lifestyle is important for overall well-being, it may not entirely prevent blood cancers. However, maintaining good health can help improve outcomes during treatment and recovery.
Arizona Oncology offers an integrated team-oriented approach to provide our leukemia and lymphoma patients with the best possible care. If you or a loved one are affected by blood cancer, remember that treatment options are constantly evolving, and support is available.

Aug 20, 2024 | Southern Arizona
August is Wellness Month and an excellent opportunity to talk about how crucial a healthy lifestyle is to cancer prevention.
Up to 90 to 95 percent of cancers have their roots in environment and lifestyle, while only 5 to 10 percent have a genetic component, according to medical oncologists at Arizona Oncology. Additionally, the World Health Organization (WHO) states that between 30% to 50% of all cancer cases are preventable.
When you make choices that prioritize your health and wellness, you are taking actionable steps against developing cancer. While not all cancer risk factors are preventable, and a healthy lifestyle is not a guarantee that you won’t ever get cancer, research has consistently shown that we do have the power to reduce our cancer risk through the lifestyle choices we make.
But before delving into what we can do, let’s take a look at actual mechanisms that fuel tumor development.
What Causes Cancer?
Cancer is a complex disease with multiple causes, including genetic, environmental, and lifestyle factors. Among the many processes that contribute to cancer development, chronic inflammation, oxidative stress, and the presence of free radicals play significant roles. These biological processes are interlinked and can create an environment that fosters the initiation, promotion, and progression of cancer.
Inflammation
Inflammation is a natural response of the immune system to injury or infection that protects us in most cases. Chronic inflammation can be damaging, as the immune cells tell the body’s cells to replace the damaged ones quickly. This constant turnover can increase the likelihood of mutations leading to the beginning of cancer.
Oxidative Stress
Oxidative stress occurs when there is an imbalance between the production of reactive oxygen species (ROS) and the body’s ability to detoxify them. ROS are chemically reactive molecules containing oxygen, including free radicals, and excessive levels can damage cellular components like DNA, proteins, and lipids. When DNA is damaged by ROS, it can lead to mutations that may result in cancer in a similar way to chronic inflammation. Moreover, oxidative stress can suppress the immune system’s ability to detect and destroy cancer cells, allowing them to proliferate unchecked.
Free Radicals
Free radicals are highly reactive atoms or molecules with unpaired electrons. They are produced naturally in the body during metabolism, but can also be introduced through environmental factors like radiation, pollution, and smoking. Free radicals can cause direct damage to DNA by inducing mutations, which are the first steps in the development of cancer. Damage to DNA can cause genes to make faulty proteins, especially in tumor suppressor genes, which help fix DNA or remove badly damaged cells. Usually, it’s a series of mutations in tumor suppressor genes and other genes that lead a cancer cell to form.
The processes of inflammation, oxidative stress, and the generation of free radicals are deeply interconnected. Chronic inflammation often leads to increased production of ROS and free radicals, further exacerbating oxidative stress. This creates a vicious cycle where oxidative damage leads to more inflammation, and inflammation generates more ROS, perpetuating cellular damage.
Environmental Factors that Are Difficult to Control, But Possible to Change
Unfortunately, environmental factors are not as easy to control as lifestyle choices. Still, it is helpful to understand which environmental factors contribute to the development of cancer. This knowledge may help you to protect yourself and also inform your choices in influencing policy decisions that affect public health.
- Air Pollution: Air pollution, caused by pollutants like PM2.5, NO2, and VOCs from vehicles, industries, and fossil fuels, can lead to respiratory and cardiovascular diseases and increase lung cancer risk. Urban areas often have high pollution levels, and while air purifiers can help, avoiding outdoor pollution is difficult.
- Radon Gas: Radon, a radioactive gas from uranium decay, can build up in buildings, especially basements, and is the second leading cause of lung cancer after smoking. It’s undetectable without special testing because it’s odorless and colorless. You can find more information about testing your home for radon gas here.
- Pesticides and Agricultural Chemicals: Pesticides and herbicides used in farming can contaminate water and food, posing cancer risks. Organic options can reduce exposure but aren’t always accessible or affordable.
- Microplastics: Tiny plastic particles from broken-down larger plastics pollute air, water, and food. They may increase cancer risk, especially in the digestive system. Reducing microplastic pollution requires global action.
- Heavy Metals: Toxic metals like lead, arsenic, and mercury, found in contaminated water, soil, and air, can cause cancers. Water filters and avoiding certain foods can help decrease your exposure, though complete avoidance is challenging due to their widespread presence.
- Endocrine Disruptors: Chemicals like BPA and phthalates, found in plastics and personal care products, can interfere with hormones and are linked to cancers such as breast and prostate. Avoiding these chemicals is difficult due to their prevalence and lack of comprehensive labeling, but you can reduce your risk by choosing BPA- and phthalate-free products.
Mitigating Cancer Risk With Healthy Lifestyle Changes
The good news is you can protect yourself from the effects of free radicals, oxidative stress, and inflammation with the lifestyle choices you make, thereby lowering your overall cancer risk. In 2024, researchers have identified the top lifestyle choices that will impact your cancer risk. They are:
- Tobacco Avoidance: Smoking is the single most preventable cause of cancer. Despite decades of public health campaigns, tobacco use continues to be a leading cause of cancer-related deaths. The ACS continues to emphasize the importance of quitting smoking and avoiding secondhand smoke as fundamental steps in cancer prevention.
- Healthy Diet and Regular Exercise: Thirty to thirty-five percent of cancers can be attributed to diet. Maintaining a balanced diet rich in fruits, vegetables, whole grains, and lean proteins, coupled with regular physical activity, can significantly lower the risk of several types of cancer, including breast, colon, and endometrial cancers. Obesity is another major cancer risk factor, with studies showing that maintaining a healthy weight is crucial in reducing cancer risk.
- Alcohol Consumption: Alcohol has been linked to an increased risk of cancers such as breast, liver, and colorectal cancer. The ACS recommends that men limit their alcohol intake to two drinks per day, and women to one drink per day.
- Vaccinations: Preventative vaccines have become increasingly important in reducing cancer risk. The Human Papillomavirus (HPV) vaccine, for example, has been shown to drastically reduce the risk of cervical cancer and other cancers linked to the virus. Research suggests that HPV vaccination might also reduce the risk of other cancers in both men and women.
- Chronic Stress Management and Mental Health: Chronic stress and poor mental health have been linked to an increased risk of cancer. The pressures of modern life, including work, education, and social factors, can contribute to higher stress levels. Chronic stress can hinder the immune system, initiate harmful hormonal changes, and encourage unhealthy behaviors (such as tobacco or alcohol use) that increase cancer risk.
- Protection From UV Exposure: UV radiation from the sun or tanning beds generates free radicals that can damage DNA and other cellular structures in the skin. When the skin’s antioxidant defenses are insufficient to neutralize these free radicals, the resulting oxidative stress can contribute to the formation of skin cancer.
Recommendations for a Cancer Prevention Diet
Besides avoiding tobacco use, research has shown that the most effective way to improve your health and reduce your risk of cancer involves your diet. A cancer prevention diet doesn’t have to be complicated or difficult to follow.
Increase Intake of Foods Rich in Antioxidants and Anti-Inflammatory Properties:
- Fruits and Vegetables: These are high in vitamins, minerals, and antioxidants such as vitamins C and E, carotenoids, and flavonoids. Examples include berries, citrus fruits, leafy greens, and cruciferous vegetables (e.g., broccoli, cauliflower, Brussels sprouts).
- Fish: Fatty fish like salmon, mackerel, and sardines are rich in omega-3 fatty acids, which have anti-inflammatory properties.
- Legumes: Beans, lentils, and peas are high in fiber and antioxidants, which can help reduce cancer risk.
- Whole Grains: Brown rice, quinoa, barley, and oats contain fiber and beneficial compounds that help lower cancer risk.
- Nuts and Seeds: Almonds, walnuts, chia seeds, and flaxseeds provide healthy fats, fiber, and antioxidants.
Avoid Foods That Increase Free Radicals and Cause Inflammation:
- Saturated Fats and Trans Fats: Found in fried foods, processed snacks, and baked goods, these fats can increase free radical production and inflammation.
- Red Meat: High consumption of red meat (beef, pork, lamb) is linked to an increased risk of colorectal cancer. Limit intake and choose lean cuts when possible.
- Sugary Drinks and Foods: Beverages and foods high in sugar can contribute to obesity and increase cancer risk. Avoid sugary sodas, candies, and desserts.
- Processed Foods: These often contain additives, preservatives, and unhealthy fats that can lead to increased free radicals and inflammation. Examples include fast food, processed meats (e.g., sausages, bacon), and packaged snacks.
Stay Active for Cancer Prevention
Regular physical activity is a key factor in reducing the risk of cancer. Health experts recommend at least 150 minutes of moderate-intensity exercise, such as brisk walking or cycling, or 75 minutes of vigorous-intensity exercise, like running or swimming, each week. It’s also beneficial to include strength training exercises at least two days a week.
Physical activity helps maintain a healthy weight, lowers inflammation, improves immune function, and regulates hormones, all of which can reduce the risk of developing cancers such as breast, colon, and endometrial cancer. Find an activity you enjoy (for example, if you find cycling boring, try pickleball), join a fitness group for accountability, park farther away from your destination, or take the stairs. Even small increases in daily activity can make a difference.
Early Detection and Screening
In addition to eating right and exercising, keeping up with your screenings is a significant way to impact your cancer risk. People of all ages should prioritize a healthy lifestyle and adhere to recommended health guidelines for screenings such as mammograms and colonoscopies.
Cancer Prevention Research is Ongoing
For the most current guidelines and information on cancer prevention, organizations such as the American Cancer Society and the American Association for Cancer Research are invaluable resources, offering detailed reports and updates on the latest advancements in the field.
Jun 19, 2024 | Southern Arizona
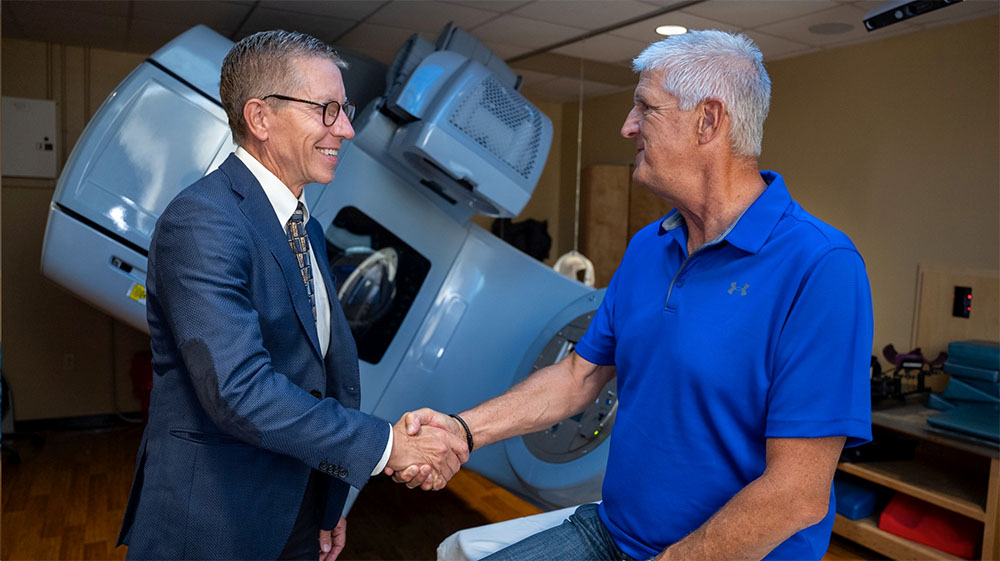
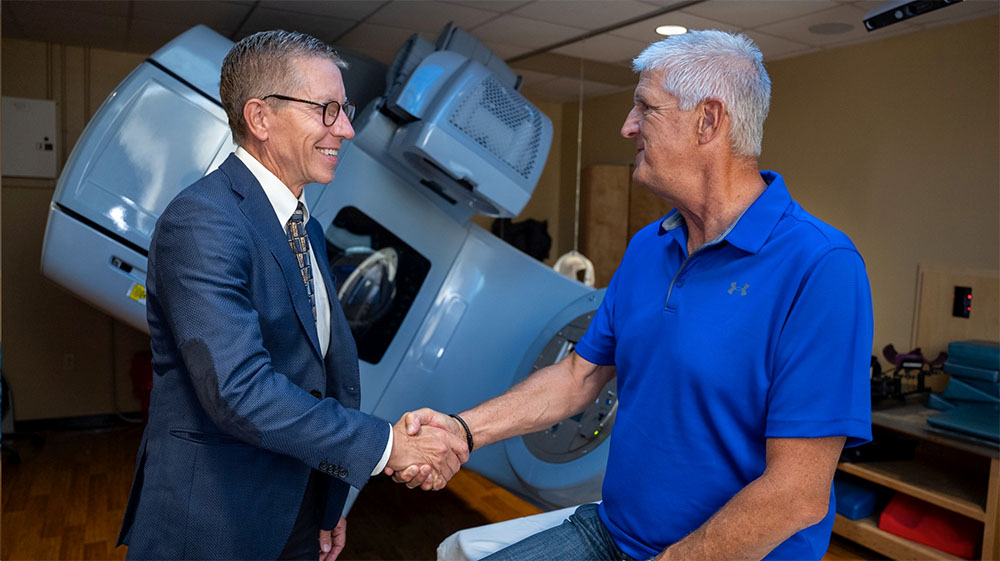
About 1 in 8 men will be diagnosed with prostate cancer during their lifetime, usually after age 65. This common cancer often grows slowly and may not cause significant harm in its early stages, but some forms of prostate cancer can be aggressive and spread rapidly to other parts of the body. This Men’s Health Month, Arizona Oncology radiation oncologist Dr. Curtis Mack weighs in on what you need to know about prostate cancer.
Starting the Journey
Have you or a loved one been newly diagnosed with prostate cancer? Prostate cancer management can follow many paths. It can be difficult to know what to do next, but you do have some control. “Start the process with your urologist to determine the stage of the disease,” says Dr. Mack. Next, he recommends setting up a consultation with a radiation oncologist and considering a second opinion from another urologist. “Knowing all your options is crucial before deciding on the best treatment plan,” Dr. Mack says.
Learn more about reading a prostate cancer pathology report and the Gleason score.
To Treat or Not to Treat
For some patients, active surveillance or “watchful waiting” is a viable option, especially if the cancer is in its early stages and not causing symptoms. Active surveillance involves regular monitoring through PSA tests, digital rectal exams, and sometimes biopsies, to keep an eye on the cancer’s progression. This approach allows patients to avoid or delay more aggressive treatments while still keeping the cancer under close observation. However, for more advanced or aggressive cancers, treatments such as surgery, radiation, or hormone therapy may be necessary. Your health care team will help you weigh the benefits and potential side effects of each treatment option to make an informed decision.
The Role of Radiation Therapy
Dr. Mack sees many prostate cancer patients, as radiation therapy is a cornerstone of prostate cancer treatment. “It has an excellent track record,” Dr. Mack says of radiation therapy for prostate cancer. Treatment is delivered externally on a daily basis or internally (called brachytherapy) using permanent or temporary radioactive seeds. Sometimes the two are combined depending on the stage of the disease and the health status of the patient. “Some of our best results are with a combination of both,” Dr. Mack adds.
Patients are often worried about side effects from prostate cancer treatment. Common short-term side effects include urinary frequency, urgency, and irritation, along with less-common gastrointestinal issues. Long-term side effects can include changes in erectile function and a small risk of urinary incontinence or leakage.
As a cancer survivor himself, Dr. Mack understands the emotions that come with undergoing cancer treatment. “I think it has made me a bit more empathetic for patients when they are going through treatment and having acute side effects, wondering if they will ever get better. I like to say that yes, they will. You just have to get through the treatment.”
Reducing Side Effects with Hydrogel Spacers
At Arizona Oncology, our use of innovations like SpaceOAR and Barrigel hydrogels have significantly reduced the side effects associated with radiation therapy for prostate cancer. These FDA-approved substances provide protection to the rectum and other nearby structures during treatment. The hydrogel is injected into the space between the rectum and prostate where the soft, gel-like material expands to create a protective space. This reduces the radiation dose delivered to the rectum.
Dr. Mack has seen the impact of these cutting-edge advancements firsthand with his patients. “SpaceOAR and Barrigel have been effective in lowering both acute and long-term radiation side effects in the rectum,” says Dr. Mack.
Women, What Does Prostate Cancer Have to Do With You?
While the emphasis may be on men’s health this month, women have a big role to play. Dr. Mack recommends that women encourage the men in their lives to keep up with prostate cancer screenings, including the PSA test. This blood test, which is often done along with a digital rectal exam, is able to detect prostate cancer at an early stage. “Screening is important,” Dr. Mack urges. “Many prostate cancers can be followed because they are early enough to undergo active surveillance but for others, the sooner we know about them, the better our treatment options and outcomes.”
If your significant other or family member has already received a diagnosis of prostate cancer, your support will be paramount. “Encourage the patient to drink plenty of fluids and remain active,” Dr. Mack recommends. “Physical activity helps with both physical and mental wellbeing.”
During Men’s Health Month, encourage your loved ones to keep up with their regular screenings, including prostate cancer screenings. Dr. Mack’s expertise reminds us that while a prostate cancer diagnosis can be daunting, understanding and exploring all options can help patients and their loved ones navigate the complex journey of prostate cancer treatment with greater confidence, clarity, and hope.

May 20, 2024 | Southern Arizona
After completing cancer treatment, you may want to take steps to help prevent a recurrence. While you cannot control every risk factor, one thing you can control is what you eat.
Nutrition plays a role in about one third of all cancers. After smoking, obesity is the most significant controllable risk factor. By maintaining a healthy weight and eating a balanced diet full of healthy, non-processed foods, you can do your part to reduce your risk.
In addition to helping prevent recurrence, a healthy, nutritious diet can also help your body recover from cancer treatment. Eating well can build strength, boost your energy levels, rebuild tissue, and help you feel better overall. Some foods can also help with treatment-related side effects. Other foods should be limited or avoided altogether.
Both the American Cancer Society and the American Institute for Cancer Research (AICR) offer recommendations for maintaining a healthy diet after cancer treatment.
Yes! Eat These Foods
- Protein is important because it provides amino acids, the essential building blocks of all living things. Protein helps build and repair tissue and make hormones and enzymes. Fill your diet with plant-based proteins like beans, lentils, soy, nuts, and quinoa. Healthy animal-based proteins include chicken, turkey, eggs, fish, and seafood. Good sources of dairy-based proteins include milk, cheese, and Greek yogurt.
- Fruits and Vegetables. These are your source of important vitamins, minerals, phytochemicals, and antioxidants, all of which work together to keep you healthy and prevent cancer. You can ensure you are getting a variety of what your body needs by choosing a mix of different colored fruits and vegetables. If your diet includes reds, greens, purples, yellows, and oranges, you’re on the right track!
- Whole grains. Whole grains are much better for you than processed grain products. Whole grains are rich in fiber, B vitamins, antioxidants, and trace minerals like zinc, iron, copper, and magnesium. Look for oats, quinoa, barley, and brown rice. Check the label for “100% whole grain” when buying bread, pasta, crackers, and cereal.
- Healthy fats are good for you! These unsaturated fats mostly come from plant sources like nuts, seeds, and avocados. Cooking oils such as canola, peanut, soybean, and olive oils are good fats, too. Fatty fish, such as salmon and sardines, are also rich in healthy fats.
- Foods rich in vitamin D and calcium. These promote bone growth and combat osteoporosis. Foods rich in vitamin D include salmon, tuna, fortified dairy products, cheese, and egg yolks. Foods rich in calcium include spinach, kale, okra, collards, soybeans, white beans, salmon, sardines, and rainbow trout.
No! Limit or Avoid These Foods
- Added sugar. There is no definitive research that sugar causes cancer, but it is well known that too much sugar isn’t good for you and is linked to obesity, which is a risk factor for cancer. Some healthy foods, like bananas, are naturally sweet. But you want to limit foods with added sugar, such as sodas, sugary cereals, granola bars, sweetened yogurts, candy, and desserts. Consume them as a once-in-awhile treat, not a daily indulgence.
- Refined carbohydrates. These are the so-called “white” foods: white bread, white rice, white flour—even regular pasta. They have been stripped of almost all fiber, vitamins, and minerals through processing, and thus are considered “empty” calories. Because they are digested quickly, they also raise your blood sugar.
- Red meat/processed meat. Red meat is associated with a higher risk of colorectal cancer, as well as other cancers. Processed meats can increase your risk of stomach and colorectal cancer. It’s best to limit or avoid these meats, which include beef, pork, lamb, lunchmeat, sausage, pepperoni, ham, and bacon.
- Trans fats. Trans fats such as partially hydrogenated vegetable oils are often found as an ingredient in commercially prepared pastries, peanut butter, fried foods, cake mix, shortening, and margarine. Eating these foods raises your levels of “bad” cholesterol and puts you at greater risk for heart disease.
- Alcohol. Studies show that alcohol is a risk factor for certain cancers. It can also make cancer treatment side effects like nausea, dehydration, and mouth sores worse. When it comes to alcohol consumption, risk increases with greater intake, but there is no drink that is “better” than another. Beer, wine, and spirits all contain ethanol, which is linked to increased cancer risk.
Build Your Healthy Plate!
The AICR recommends following as much of a plant-based diet as possible. A good start is to follow the New American Plate for cancer prevention.
The New American Plate states:
- At least 2/3 of your plate should be covered with plant-based foods like vegetables, whole grains, fruit, and beans.
- Up to 1/3 of your plate can contain animal-based protein-rich foods like seafood, poultry, dairy, and the occasional lean red meat.
Other AICR recommendations include:
- Eat at least 30g of fiber per day
- Eat at least 3.5 to 5 cups of fruits and vegetables each day
- Be a healthy weight
- Be physically active
- Limit processed, “fast” foods that are high in starches, sugars or fat
- Eat no more than 12-18 ounces per week of red meat
- Avoid processed meat
- Drink mostly water; avoid sweetened beverages
- Limit or avoid alcohol altogether
- Focus on getting your nutrition from food, not supplements
- Mothers should breastfeed their babies if possible; it reduces breast cancer risk
- Cancer survivors should talk to their doctors about nutritional recommendations
Last, but not least, it bears repeating that avoiding tobacco is the number one thing you can do to reduce your cancer risk. Resources to help you quit can be found here.

May 12, 2024 | Southern Arizona
Is Melanoma Genetic?
Melanoma is the most dangerous type of skin cancer. It forms in the cells that produce melanin, which is the substance responsible for your skin’s color. Exposure to ultraviolet radiation (UV rays) from the sun or tanning beds increases the risk of developing any skin cancer. In the case of melanoma, experts say there’s also a strong link between genetics (your family history) and your risk of developing melanoma.
Family History and Genetic Factors
If one or more of your parents, siblings or children develop melanoma, you have a higher risk of developing melanoma than a person with no family history of the disease. Experts aren’t sure whether the increased risk is because close relatives tend to have similar lifestyles (such as spending lots of time outside in the sun together) or if a genetic mutation is responsible. Regardless of why a family history of melanoma raises the risk of developing the disease, knowing that there’s a link means you should take precautions. That can include reducing the skin cancer risk factors you can control and paying close attention to changes in your skin.
Am I at Risk for Melanoma?
Everyone is at risk for melanoma, regardless of family history. Some people with a family history of the disease never get it. Some people with no family history will get it.
Fortunately, there are concrete steps you can take to reduce your melanoma risks, including:
Did you know sunscreen can expire? Check the date and do not use if it’s expired!
- Avoiding tanning beds.
- Limiting your time outdoors when the sun’s rays are strongest (between 10 am and 4 pm).
- Applying sunscreen of SPF 30 or higher liberally 15-30 minutes before any sun exposure and reapplying every 2 hours throughout the day, after toweling, becoming sweaty or getting wet.
- Checking the expiration date of your sunscreen – do not use if it’s expired.
- Following directions for sunscreen application on babies less than 6 months old.
- Wearing protective clothing, hats and sunglasses so sunlight can’t reach your skin.
Early Detection Increases Survival Rates for Melanoma
Melanoma is responsible for 75% of all skin cancer deaths. A person’s risk of dying from melanoma increases the deeper the cancer grows. Melanomas that aren’t detected early and are allowed to grow can spread to other parts of the body, and because melanoma is an aggressive cancer, it spreads quickly – usually within three to 18 months from the time it becomes noticeable.
Frequent skin exams are especially important for people with a family history of melanoma. Once a melanoma has spread (doctors use the term “metastasized”), the cancer is much more difficult to treat. That’s why it’s so important for everyone to examine their skin and have their skin examined regularly by a doctor. These exams give you and your doctor an opportunity to spot suspicious growths on the skin early. A melanoma that is found early can be removed from the skin before it is able to spread.
Skin Self Exams: What to Look For
Examining your skin monthly allows you to become familiar with the location and appearance of your freckles, moles and other pigmented areas. Whenever you detect changes to existing marks on your body, or new growths or pigmented areas that look unusual or are growing quickly, you should have them checked out by a dermatologist.
Doctors recommend remembering the ABCDEs of melanomas when you’re checking your skin:
- Asymmetry. If you draw an imaginary line through the middle of a melanoma, the two halves would not match.
- Border. The edges of a melanoma are usually uneven, fuzzy or jagged.
- Color. Melanomas change colors and are often a combination of black, brown and tan.
- Diameter. Melanomas may grow larger than the size of a pencil eraser.
- Elevation. Once a mark on your skin becomes raised or thicker, it is a serious red flag indicating a melanoma may be spreading and should be evaluated by a doctor immediately.
Melanoma can be deadly. Whether you have a family history of the disease or not, you’re at risk. Get to know your skin so you’ll know when something simply doesn’t seem right, and if you notice any changes of your skin, it is best to visit your doctor or dermatologist. Arizona Oncology has locations throughout the state if your provider determines a referral is needed.
Originally posted in 2017, updated in 2024.

May 11, 2024 | Southern Arizona
Prostate cancer research has been an ongoing process of looking into causes, prevention, detection, and treatment of prostate cancer. But with hundreds upon hundreds of published studies out there, how can patients keep up with what’s new? Here are some recent developments to watch in prostate cancer treatment:
1. Genetic & Genomic Testing Related to Prostate Cancer
Genes can play a role in both the development and behavior of prostate cancer. Two types of tests that can be helpful in acquiring information are genetic testing and genomic testing. While they sound similar, they collect different information.
- Genetic testing is used more frequently to define high-risk populations who have yet to get cancer. People who have a known family history of cancer may want to investigate further with genetic testing to see if they carry a gene mutation that puts them at risk. New research on gene changes linked to prostate cancer is helping scientists better understand how prostate cancer develops.
- Genomic testing, on the other hand, is done for patients who have been diagnosed with prostate cancer in hopes of determining how the cancer might behave. This information can be beneficial in deciding the course of care for your cancer. Some of the genomic tests available now include Decipher, Oncotype DX, ProstaVysion, and the Prolaris Test.
Depending on a patient’s circumstance, a doctor may recommend either test if it could be beneficial to the detection of an inherited risk for or the treatment of prostate cancer.
2. Immunotherapy
The goal of immunotherapy is to boost the body’s immune system to help fight off or destroy cancer cells. Prostate cancer has seen much promise and potential in changing the way this disease is treated and cured in the field of immunotherapy.
Prostate cancer immunotherapy studies are being conducted in the following seven categories:
- Therapeutic vaccines: intended to treat or cure a disease by stimulating the immune system
- Oncolytic virus therapies: intended to kill cancer cells and stimulate an immune response against tumors
- Checkpoint inhibitors: drugs that block normal proteins on cancer cells, or the proteins on the T-cells that respond to them
- Adoptive cell therapies: the collection of T-cells from the blood, which are then modified, and injected back into the patient so they can better recognize cancer cells in the body
- Adjuvant immunotherapies: substances used to boost the immune system so the patient’s response to therapeutic vaccines can be improved
- Cytokines: the injection of laboratory-produced cytokines (proteins that boost the immune system) to increase the number of ones the body would normally produce
- Monoclonal antibodies: antibodies designed in a lab that specifically target a certain antigen, such as one found on cancer cells
According to the American Cancer Society, one promising approach for the future might be to combine a checkpoint inhibitor with a prostate cancer vaccine. This combination could strengthen the immune response and help a cancer vaccine work better.
3. Earlier Detection
Researchers are trying to develop a better prostate-specific antigen (PSA) test, which could lead to earlier prostate cancer detection (PSA is a protein that is produced exclusively by prostate cells. An overabundance of this protein may indicate that cancer is present).
Additionally, cancer researchers are developing a urine test to find a gene called prostate cancer gene 3 (PCA3), which could also help detect prostate cancer more quickly. When a man has prostate cancer, PCA3 is made in larger amounts when a man has prostate cancer. More accurate testing could help prostate cancer doctors decide if a man needs a prostate biopsy. With a better testing method, more healthy men could be screened for prostate cancer, resulting in prostate cancers being found and treated early.
Thirdly, imaging with PSMA PET is far more sensitive than combinations of bone scan and CT imaging to detect prostate cancer spread, to assist staging, and to dictate treatment alterations.
4. Stereotactic Body Radiation Therapy (SBRT)
Stereotactic Body Radiation Therapy (SBRT) is a highly targeted form of radiation treatment that delivers precise, high doses to tumors while minimizing damage to surrounding healthy tissue. Radiation therapy using SBRT can be used to treat patients whose cancer has spread to five or fewer sites. This treatment can help keep the cancer from recurring and may also delay the need for hormone therapy.
5. The Approval of Pluvicto
Pluvicto is a targeted radioligand therapy for advanced prostate cancer that binds to cancer cells and delivers radiation directly to them, helping to slow disease progression and manage symptoms. It is an option for patients with castrate-resistant prostate cancer with spread who have not had success with other treatments.
Most new research is developed through prostate cancer clinical trials. Prostate cancer research trials are designed to test new ways to prevent, find, diagnose, treat, and manage the disease more effectively.
Arizona Oncology has recently participated in a variety of prostate cancer clinical trials and has another exciting one on the horizon. Don’t hesitate to speak with your prostate cancer specialist today about the possibility of joining a prostate cancer clinical trial.
Originally posted in 2018. Updated in 2024.
Page 3 of 18«12345...10...»Last »